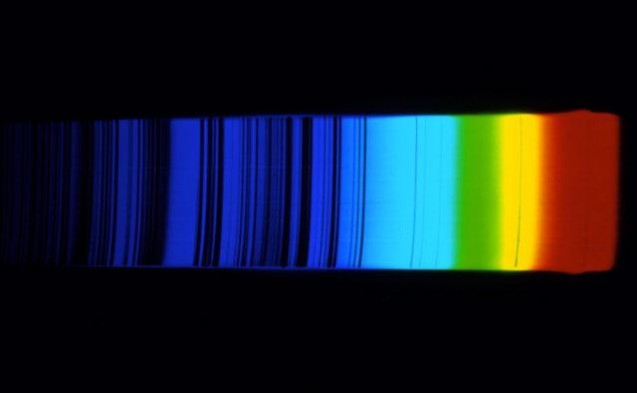
The use of near-infrared (NIR) spectroscopy as an adjunct to morphology for metabolomic profiling of culture media for selecting embryos does not improve the live birth rate significantly in comparison to embryo selection by morphology alone, states a multi-center study.
Proof of principle studies have suggested the use of the NIR and the derivation of a viability score as a tool for assessing embryo viability (Seli et al., 2007, 2010, 2011; Nagy et al., 2008, 2009; Scott et al., 2008; Vergouw et al., 2008, 2011; Ahlstrom et al., 2011). In 2012, Vergouw et al. conducted a double-blind RCT that showed Day 3 embryo selection by metabolomic profiling of culture medium with NIR spectroscopy as an adjunct to morphology did not improve ongoing pregnancy and live birth rates compared with morphology alone.
However, Sfontouris et al. (2013) found significantly higher ongoing implantation rates for Day 5 transfers, but similar ongoing pregnancy and live birth rates, in their RCT in which embryo selection by metabolomic profiling with NIR spectroscopy plus morphology was compared with morphology alone; however, that study was terminated early and therefore lacked adequate power.
The purpose of the current study by C.G. Vergouw and colleagues was to utilize individual patient data meta-analysis (IPD MA) to assess the efficacy of metabolomic profiling of culture medium with NIR spectroscopy technology as an adjunct to embryo morphology in IVF. “The IPD MA indicates that the live birth rate after embryo selection by NIR spectroscopy and morphology is not significantly different compared with the live birth rate after embryo selection by morphology alone,” wrote Vergouw et al. (“No evidence that embryo selection by near-infrared
spectroscopy in addition to morphology is able to improve live birth rates: results from an individual patient data meta-analysis,” HR, 2014;29(3):455-461).
Included studies were those that reported results of an RCT comparing embryo selection by morphology to embryo selection by morphology and use of NIR spectroscopy of spent embryo culture medium. A literature search was performed in PubMed, the Cochrane Library, and the WHO International Clinical Trials Registry using relevant terms. Selected studies utilized a randomized design with a population of women who underwent IVF or ICSI treatment.
Authors of eligible studies were asked to send in their data set, from which data relevant to the current study were obtained. Study quality of selected studies was independently assessed by two authors using the Cochrane checklist for evaluation of RCTs (Dutch Cochrane Collaboration, 2012).
Statistical analysis utilized SAS Proc Glimmix, SPSs 20.0, and STATA 12 software and included intention-to-treat (ITT) analysis, testing by the I ² statistic in a random effects model, and logistic regression analysis. Four RCTS were identified as eligible for inclusion in the present IPD MA; four databases were obtained (Hardarson et al., 2012; Vergouw et al., 2012; Sfontouris et al., 2013; Economou, no date given), three of which had been published previously (Hardarson et al., 2012; Vergouw et al., 2012; Sfontouris et al., 2013).
Study size of original clinical trials varied between 55 and 417 patients (ITT population); the four databases combined included 924 IVF/ICSI cycles of 924 patients. The control group was made up of 484 patients for whom embryos for transfer were selected by morphology alone, while the treatment group was made up of 440 patients for whom embryos were selected by morphology
plus NIR spectroscopy. Data regarding live birth was available for all 924 patients.
For the control group, the live birth rate was 34.7% (168 of 484), while that of the NIR group was 33.2% (146 of 440). The results of the IPD MA logistic regression analysis gave a pooled odds ratio (OR) of 0.98 [95% confidence interval (CI) 0.74 - 1.29], which indicated the live birth rates did not differ significantly between the two groups. Data of the four studies showed no significant
heterogeneity; consequently, a fixed effect model was applied in the IPD MA.
The following variables were used for model building and evaluation of potential confounders (all were provided by all four studies): maternal age, medical cause of infertility, number of previous IVF attempts, treatment type, number of oocytes at OPU, fertilization method, number of fertilized oocytes, number of good quality embryos, number of embryos transferred, and day of
embryo transfer. The test for interaction effects of the treatment group with all potential confounding variables was not significant. The strongest confounding factors were: maternal age, medical cause of infertility, number of previous IVF attempts, number of oocytes at OPU, and number of fertilized oocytes. Multivariable logistic regression analysis including these confounding variables showed the study group was not related to live birth (OR 0.97, 95% CI 0.73 - 1.29).
“There is at present no evidence that NIR spectroscopy of spent embryo culture media in its current form can be used in daily practice to improve birth rates,” concluded Vergouw et al.
Address correspondence to C.G. Vergouw, Department of Obstetrics and Gynecology, VU University Medical Center, Amsterdam, The Netherlands; e-mail: carljin.vergouw@vumc.nl.
More
Failure to conceive following fertility evaluation leads to a significantly higher likelihood of divorce or end of cohabitation, state researchers in Denmark.
Infertility is a source of stress that impacts the couple physically, psychologically, and socially (Schmidt, 2006; Verhaak et al., 2007). When fertility treatment fails to produce a pregnancy, the couple may experience decreased quality of life (Hammarberg et al., 2001; Johansson et al., 2009) and increased stress, anxiety, and depression (Verhaak et al., 2005, 2007). Couples struggling with fertility problems may also experience sexual (Wischmann, 2010) and marital distress resulting from differences in coping strategies and communication (Hielmstedt et al., 1999; Chachamovich et al., 2010; Peterson et al., 2009; Monga et al., 2004).
There is little available data on the likelihood of divorce or end of cohabitation in the long term when couples fail to conceive.
To gain further understanding of the above, Trille Kjaer and colleagues performed a study in which they investigated the likelihood of divorce or end of cohabitation for couples who fail to conceive after fertility evaluation (“Divorce or End of Cohabitation Among Danish Women Evaluated for Fertility Problems,” Acta Obstet Gynecol Scand, 2014;93:269-276). “Parity after a fertility evaluation may be an important component in the longitudinal relationships of couples with fertility problems,” wrote Kjaer et al.
This longitudinal cohort study included 47,515 Danish women who had been referred for primary or secondary fertility problems between 1990 and 2006. The information was linked to Danish administrative population-based registries, which contained demographic and socioeconomic data. Discrete-time survival models were used with person-period statistics.
Each woman was followed from one year after her fertility evaluation through 2007. The primary outcome measure was the effect of parity after a fertility evaluation on the likelihood of divorce or end of cohabitation.
After as much as 12 years of follow up, almost 27% of the women were divorced or no longer living with the partner they were living with at the time they underwent fertility evaluation.
Women who did not have a baby following fertility evaluation had a considerably higher odds ratio for ending their relationship up to 12 years following the evaluation (with odds ratios up to 3.13, 95% CI 2.88-3.41) compared to women who had a baby, in spite of their parity prior to the evaluation.
“In conclusion, women evaluated for fertility problems who did not have a child after an initial evaluation had significantly higher Ors for divorce or end of cohabitation in the first 12 years after the evaluation, regardless of their parity before the evaluation,” stated Kjaer et al.
“These findings suggest that not having a child after a fertility evaluation seems to be an important component in
the longitudinal relationships of couples with fertility problems.”
Address correspondence to Trille Kristina Kjaer, Department of Survivorship, Danish Cancer Society Research Center, Strandboulevarden 49, 2100 Copenhagen O, Denmark; E-mail:trille@cancer.dk
More
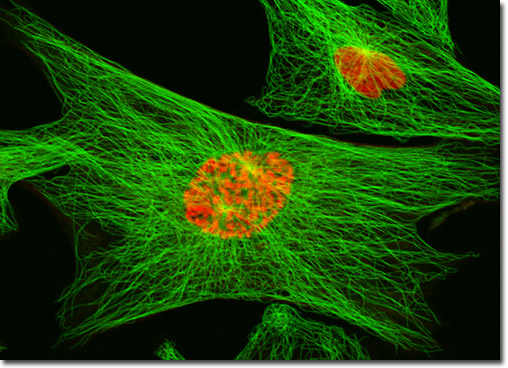
Human early follicle growth in vitro is improved with the addition of basic fibroblast growth factor (bFGF), according to research from China.
bGb takes part in follicle development. Mammal studies have documented expression of bFGF and its receptors in early ovarian follicles in rat (Nilsson et al., 2001), goat (Wandji et al., 1992), cow (van Wezel et al., 1995) and human (Yeh and Osathanondh, 1993; Quennell et al., 2004; Ben-Haroush et al., 2005).
In human ovarian tissue culture, bGFG reportedly plays a role in estrogen production by the ovarian cortex, and high doses of bFGF improve primordial follicle development (Garor et al.,2009).
A recent study by Gao et al. (2013) found that bFGF may significantly improve quality of transplanted ovarian tissues.In the current study, researchers T. Wang and colleagues sought to determine the effects of bFGF on growth of individual early human follicles in a three-dimensional (3D) culture system
in vitro.
“The addition of 200 ng bFGF/ml improves human early follicle growth, survival and viability during growth in
vitro,” stated Wang et al. (“Basic fibroblast growth factor promotes the development of human ovarian early follicles during growth in vitro,” HR, 2014;29(3):568-576).
Ovarian tissue samples were obtained from 11 women undergoing laparoscopic surgery for gynecological disease. Follicles were isolated from fresh tissue as previously described (Vanacker et al., 2011). Follicles were encapsulated in a 1% alginate bead as previously described (Xu et al., 2006a, b), with some modifications.
Follicles were randomly divided into four study groups and transferred to basic culture media supplemented with bFGF 0, 100, 200, or 300 ng/ml. Half of the culture media was replaced every 2 days and morphology of
follicles was analyzed and diameter was measured.
Fresh culture media was prepared weekly. Follicles were observed, photographed, and had diameters calculated. Growth and survival data were reported on Day 8 of culture. Follicles were considered to be surviving unless they had dark oocytes and/or granulosa cells (GCs) or had no integrity between the oocyte and the GCs (Xu et al., 2009b). Early follicular stages were classified into four types based on descriptions by Gougeon (1996) and Fortune (2003): primordial follicle, primary follicle, secondary follicle, and pre-antral follicle. Follicles were incubated with fluorescent dyes (Cortvrindt and Smitz, 2001), washed, and examined under a microscope. Follicles were then classified into four categories based on the presence of dead GCs: Viability I (V1), live follicles; Viability 2 (V2), minimally damaged follicles; Viability 3 (V3), moderately damaged follicles; Viability 3 (V3), moderately damaged follicles; Viability 4 (V4), dead follicles (Dolmans et al., 2006).
Statistical analysis utilized SPSS 18.0 software and included Kruskal-Wallis test and MannWhitney tests with post
hoc tests, as required. P < 0.05 was considered significant.
In total, 154 follicles were cultured, all of which increased in size after 8 days. Initial mean diameters in groups cultured with 0 ng/ml bFGF (n = 38), 100 ng/ml (n = 42), 200 ng/ml (n = 39) and 300 ng/ml bFGF (n = 35) were 75.9 ± 20.4, 76.4 ± 22.9, 77.9 ± 20.1, and 74.6 ± 23.1 µm, respectively. No significant differences were noted in size among the four groups. At the end of Day 8, follicular sizes for bFGF 0, 100, 200 and 300 ng/ml groups had increased to 90.2 ± 29.8, 117.3 ± 42.5, 133.3 ± 35.1, and 110.0 ± 39.2 µm, respectively. Diameter in the group 200 ng/ml bFGF on Day 6 and 8 (128.4 ± 35.2 and 133.3 ± 35.1 µm) was significantly (P < 0.05) higher than that of the group of 0 ng/ml bFGF (88 ± 22.8 and 90.2 ± 29.8 µm).
bFGF culture also promoted follicle survival. Survival rate of follicles in the 0 ng/ml bFGF group was 36.8% at Day 8, but survival rates for those in the 100, 200, and 300 ng/ml bFGF groups increased significantly to 73.8, 76.9, and 65.7%, respectively. After 8 days in IVC, a significantly higher number of follicles had activated and differentiated into advanced follicle stages in the 200 ng/ml group compared to the 0 ng/ml bFGF group (P < 0.05).
Ninety-eight isolated human follicles were examined for viability on Day 8. Viability was significantly (P < 0.05) higher in the 200 ng/ml bFGF group with 77.2% V1 and V2 (13.6% + 63.6%, respectively) compared to that of the 0 ng/ml bFGF group with 16.7% V1 and V2 (0% + 16.7%, respectively). Poor quality follicles (V3 + V4) accounted for 83.3% in the 0 ng/ml bFGF group, with 41.7% dead follicles (V4); while in the group of 200 ng/ml bFGF, V3 + V4 accounted for 22.7%, with 9.1% of dead follicles (V4) (P < 0.05).
In concluding their study, Wang et al. wrote, “We have shown that the growth of human follicles at early stage can be promoted by bFGF in 3D system.”
Address correspondence to Jie Qiao, Department of Obstetrics and Gynecology, Peking University Third Hospital, No. 49 Hua Yuan Bei Road, HaiDian District, Beijing 100191, China; e-mail: jie.qiao@263.net.
More